Impact on Other Parts of the Body
Cystic fibrosis (CF) impacts other parts of the body as well. This can be caused by the progression of the disease or the effects of necessary medicines used to treat it. Keep in mind that everyone with CF experiences progression but not everyone’s CF progresses in the same way.
Cystic fibrosis (CF) impacts other parts of the body as well. This can be caused by the progression of the disease or the effects of necessary medicines used to treat it. Keep in mind that everyone with CF experiences progression but not everyone’s CF progresses in the same way.
Cystic fibrosis (CF) impacts other parts of the body as well. This can be caused by the progression of the disease or the effects of necessary medicines used to treat it. Keep in mind that everyone with CF experiences progression but not everyone’s CF progresses in the same way.
Impact on the Pancreas
The pancreas does 2 important jobs. It makes enzymes that break down the fats and proteins in food. It also makes hormones, such as insulin, which help regulate blood sugar levels. As CF progresses, it can limit the pancreas' ability to do these jobs.
Pancreatic insufficiency
In people with CF, thick fluids block small tubes in the pancreas called ducts. This blockage makes it harder for the enzymes to reach the small intestine where they help digest food. Not having a sufficient amount of these digestive enzymes in the small intestine is called pancreatic insufficiency.
85% to 90% of people with CF have pancreatic insufficiency (PI), which is common even at a young age.
85% to 90% of people with CF have pancreatic insufficiency (PI), which is common even at a young age.
85% to 90% of people with CF have pancreatic insufficiency (PI), which is common even at a young age.
Pancreatitis
The small group of patients that remain pancreatic sufficient may experience a condition called pancreatitis. Pancreatitis is inflammation of the pancreas, and it can result in severe symptoms such as abdomen and back pain, nausea, vomiting, fever, rapid pulse, and weight loss.
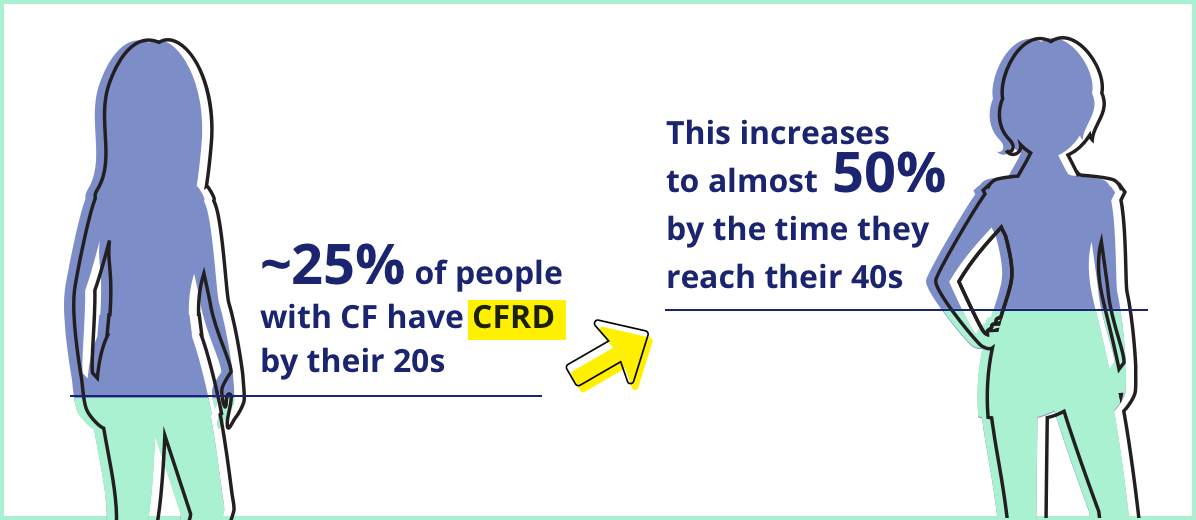
The pancreas: cystic fibrosis-related diabetes (CFRD)
Over time, scarring in the pancreas, caused by thick digestive fluids, can damage the cells that produce insulin. Insulin is a hormone that is essential to regulating blood sugar.
Some people with CF can develop CFRD, a form of diabetes seen in people with CF. CFRD is when the pancreas doesn't make enough insulin. When acutely ill, the body may not properly use the insulin it does produce. As a result, blood sugar levels will increase.
Some people with CF can develop CFRD, a form of diabetes seen in people with CF. CFRD is when the pancreas doesn't make enough insulin. When acutely ill, the body may not properly use the insulin it does produce. As a result, blood sugar levels will increase.
Some people with CF can develop CFRD, a form of diabetes seen in people with CF. CFRD is when the pancreas doesn't make enough insulin. When acutely ill, the body may not properly use the insulin it does produce. As a result, blood sugar levels will increase.

STAY CF SMART: According to the American Diabetes Association, annual screening for CFRD should begin by age 10 in all people with CF who do not have CFRD.
STAY CF SMART: According to the American Diabetes Association, annual screening for CFRD should begin by age 10 in all people with CF who do not have CFRD.
STAY CF SMART: According to the American Diabetes Association, annual screening for CFRD should begin by age 10 in all people with CF who do not have CFRD.
CFRD is a serious condition. The symptoms are often similar to CF or are not noticeable. If CFRD is left untreated, CF symptoms can worsen and the effects of chronic high blood sugar can lead to:
- Reduced ability to fight infection
- Muscle loss
- Weight loss
- Liver disease
- Nerve problems
- Complications in the kidneys
- Decline in vision
Note that CFRD is different from type 1 and type 2 diabetes and, therefore, is treated differently.
Impact on the Liver
Liver disease is considered to be one of the most serious health risks associated with CF. People with CF have thicker bile, and as a result, the tubes that drain bile—bile ducts—can become blocked. This often leads to irritation or inflammation in the liver.
Over time, thick bile can lead to scarring and damage of the liver, which can cause a condition called cirrhosis. Keep in mind that cirrhosis occurs in the late stages of CF-related liver disease and not everyone with CF-related liver disease experiences it.
Cirrhosis makes it difficult for blood to travel through the liver. It can cause many complications, including:
- Low blood counts
- Fluid buildup in the abdomen
- Bleeding in the esophagus
- Difficulty breathing
About 10% to 20% of people with CF develop liver disease, which includes cirrhosis, a buildup of fat in the liver, hepatitis, and other complications.
About 10% to 20% of people with CF develop liver disease, which includes cirrhosis, a buildup of fat in the liver, hepatitis, and other complications.
About 10% to 20% of people with CF develop liver disease, which includes cirrhosis, a buildup of fat in the liver, hepatitis, and other complications.

STAY CF SMART: Care teams regularly monitor liver function in people with CF to check for CF progression in the liver because there are often no symptoms until the damage reaches an advanced stage.
STAY CF SMART: Care teams regularly monitor liver function in people with CF to check for CF progression in the liver because there are often no symptoms until the damage reaches an advanced stage.
STAY CF SMART: Care teams regularly monitor liver function in people with CF to check for CF progression in the liver because there are often no symptoms until the damage reaches an advanced stage.
Both CFRD and cirrhosis are serious complications of CF.

Scarring in the pancreas and the liver, caused by thick digestive fluids over time, can lead to serious complications such as CFRD and cirrhosis, respectively. Learn More >
Impact on the Bones
For people with CF, different factors contribute to low bone density, a condition where bones become less dense and are not as strong as they should be. Some people with CF may lose bone density more easily. Low bone density is sometimes referred to as osteopenia, and when severe, osteoporosis.
For people with CF, bone health may be affected because they often have trouble absorbing enough vitamin D. Another factor contributing to low bone density is the increased inflammation throughout the body that is made worse by frequent lung infections. This may cause bones to be weak and less dense. Therefore, they can fracture more easily. These factors can contribute to both osteopenia and osteoporosis.

STAY CF SMART: Care teams begin screening people with CF for bone health at an early age and may suggest using vitamin D supplementation.
STAY CF SMART: Care teams begin screening people with CF for bone health at an early age and may suggest using vitamin D supplementation.
STAY CF SMART: Care teams begin screening people with CF for bone health at an early age and may suggest using vitamin D supplementation.
Up to 26% of adults with CF may have
low bone density.
Up to 26% of adults with CF may have
low bone density.
Up to 26% of adults with CF may have
low bone density.
Some effects of CF may have no symptoms.

Many effects of CF are silent at first. For example, lung damage may be occurring before it can be detected by some tests. Learn More >
Impact on the Kidneys
CF does not directly affect the kidneys, however, about 2% of people with CF between the ages of 25 and 35 have chronic kidney disease (CKD). There are 3 risk factors that make adults with CF at risk for CKD:
- Treatments with certain necessary medicines
- Treating other CF-related conditions with medicines such as antibiotics for an extended period of time can affect the kidneys
- Progressive cystic fibrosis-related diabetes (CFRD)
- High blood sugar in people with CFRD can over time lead to CKD
- Kidney stones
- Kidney stones form as a result of an accumulation of minerals inside the body that is caused by how the digestive system of a person with CF absorbs minerals. Kidney stones can cause pain and blood in urine
Impact on Hearing
Although CF does not directly impact hearing, medications and treatments that are extremely important for people with CF can damage hearing over time. Hearing loss is common in people with CF who have been exposed to certain medications such as aminoglycosides for an extended period of time.

People with CF who receive certain necessary antibiotics may experience a 20% loss in hearing.
People with CF who receive certain necessary antibiotics may experience a 20% loss in hearing.
People with CF who receive certain necessary antibiotics may experience a 20% loss in hearing.

STAY CF SMART: It’s important to discuss the progression of hearing loss with the care team so they can help.
STAY CF SMART: It’s important to discuss the progression of hearing loss with the care team so they can help.
STAY CF SMART: It’s important to discuss the progression of hearing loss with the care team so they can help.